Statins are among the most commonly prescribed drugs in the world. They are used for their ability to lower cholesterol and reduce the risk of cardiovascular disease. For so many men, a routine doctor’s visit will end with a prescription for statins – often without much discussion of alternatives or any mentions of lifestyle interventions, root causes, etc. But are these medications always necessary, or are we overprescribing them at the expense of men’s overall health?
The numbers don’t lie: over 92 million Americans are on statins, and the majority of those are men, even in cases where lifestyle changes could achieve similar results. This blog takes a look into the growing concerns around the potential overprescription of statins, their side effects, and the alternatives that might better serve men striving for long-term health.

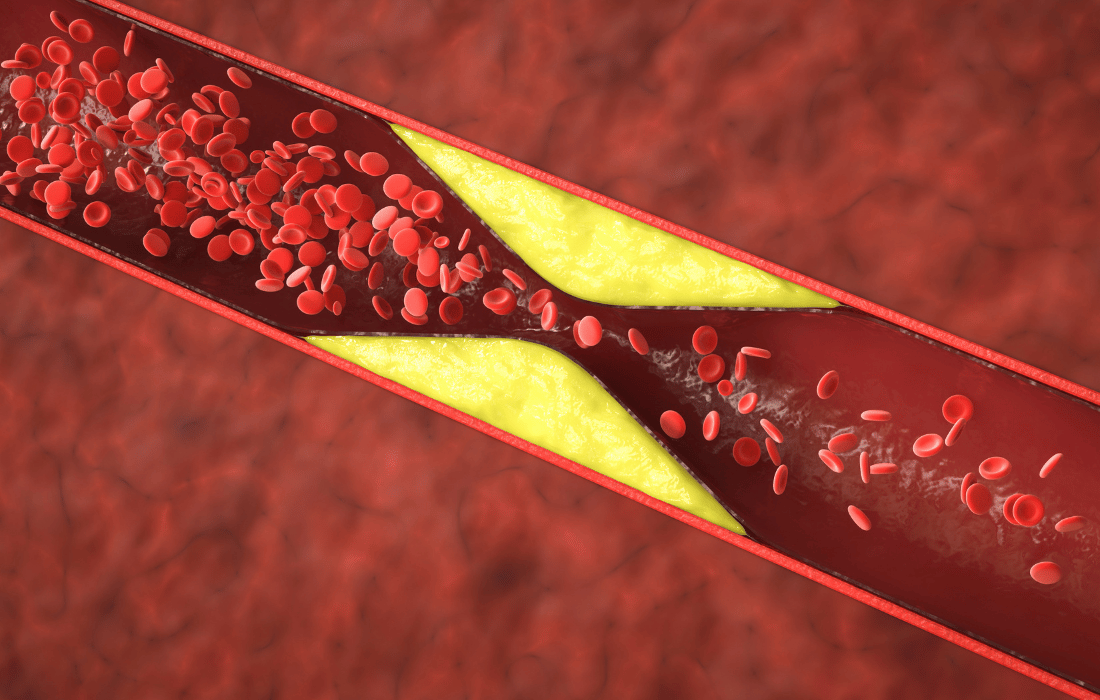
What Are Statins and How Do They Work?
Statins work by blocking an enzyme in the liver responsible for producing cholesterol, particularly LDL (low-density lipoprotein), often referred to as “bad cholesterol”. Lowering LDL cholesterol can reduce the risk of heart attacks and strokes, making statins a go-to medication for those with cardiovascular disease or high cholesterol levels.
However, statins are also prescribed preventively to millions of men who may not be at that high of risk. According to recent data, nearly 1 in 4 Americans over 40 takes a statin. Among men, the rates are even higher, with many beginning treatment simply because their cholesterol numbers exceed an arbitrary statistic-based threshold.
The Problem with Overprescription
While statins have undoubtedly saved lives, their widespread use raises questions about whether they’re prescribed too liberally. Current guidelines often recommend statins based on risk calculators that include age, blood pressure, and cholesterol levels. But these calculators don’t always account for individual circumstances, such as diet, exercise habits, or genetic predispositions.
Broad Criteria, Narrow Benefits
The criteria for prescribing statins have expanded over the years, partly driven by pharmaceutical companies that benefit from higher sales. Some experts argue that the thresholds for “high cholesterol” are too low, pushing many men into treatment when their risk of heart disease might be minimal. This raises concerns about the medicalization of otherwise healthy individuals.
Real-Life Implications
Consider a 45-year-old man with slightly elevated cholesterol but no family history of cardiovascular issues. He’s active, eats well, and doesn’t smoke. Despite his overall health, he might still be prescribed statins as a precaution. This one-size-fits-all approach can lead to unnecessary medication, potential side effects, and a false sense of security that medication alone is enough.

Potential Risks and Side Effects
Like any medication, statins come with risks – some of which can have a significant impact on a guy’s health and quality of life.
Common Side Effects
Many men experience muscle pain, fatigue, or weakness while taking statins. These side effects can discourage physical activity, undermining one of the most effective ways to improve heart health naturally. Liver damage, while rare, is another potential concern.
Long-Term Risks
More troubling are the less-publicized risks:
- Cognitive Issues: There have been reports that statins may impair memory or contribute to brain fog in certain individuals, although the research is far from clear or conclusive.
- Increased Risk of Diabetes: Research shows that statin use, particularly at high doses, can increase the likelihood of developing type 2 diabetes.
- Testosterone Suppression: Cholesterol is a building block for testosterone production. Lowering cholesterol too much can potentially impact hormone levels, affecting libido, muscle mass, and energy.
These risks show us the importance of weighing the benefits of statins against their potential drawbacks, particularly in those with moderate risk factors who might not need medication at all.
The Alternatives to Statins
For many men, lifestyle changes can be just as effective as medication in managing cholesterol and reducing cardiovascular risk. Here’s what works:
- Dietary Adjustments
-
- Reduce intake of refined carbohydrates and trans fats.
- Focus on heart-healthy foods like fatty fish, nuts, seeds, and leafy greens.
- Incorporate more soluble fiber, which can help lower LDL cholesterol.
- Exercise
-
- Engage in regular cardiovascular and strength training activities to improve heart health and maintain muscle mass.
- Even 30 minutes of brisk walking daily can significantly lower cardiovascular risk.
- Stress Management

-
- Chronic stress contributes to inflammation, which plays a role in heart disease. Practices like meditation, yoga, or even hobbies can help.
- Quality Sleep
-
- Poor sleep is linked to higher cholesterol levels and heart disease. Aim for 7-9 hours of restorative sleep per night.
The Importance of Individualized Care
One of the biggest issues with statin overprescription is the lack of personalized care. Risk calculators and lab results are helpful tools, but they don’t tell the whole story. Factors like family history, lifestyle habits, and even mental health should play a role in deciding whether statins are necessary.
Men need to be empowered enough to question their prescriptions and advocate for individualized care. A good doctor should discuss alternatives and lifestyle factors, monitor progress, and reassess the need for medication over time. If you’re prescribed statins, ask questions like:
- Do I really need this medication?
- What are the potential side effects, and how can we manage them?
- Are there lifestyle changes I can try first?

When Are Statins Necessary?
It’s important to acknowledge that statins can be life-saving for men at high risk of cardiovascular events. For example, someone with a history of heart attack or stroke or severely elevated LDL cholesterol levels may benefit greatly from these medications.
However, even in these cases, monitoring and minimizing side effects is essential. Statins should be part of a comprehensive plan that includes diet, exercise, and other lifestyle interventions.
Conclusion
Statins certainly have their place in modern medicine, but their overprescription raises serious questions about the medicalization of men’s health. For many, addressing the root causes of high cholesterol – diet, exercise, stress, and sleep – can achieve similar results without the risks of medication.
Guys need to take an active role in their healthcare, questioning whether a prescription is truly necessary, advocating for alternatives when appropriate, and cultivating genuine health through their daily habits. By focusing on holistic health rather than quick fixes, we can reduce our dependence on medication and build a stronger foundation for long-term wellness.