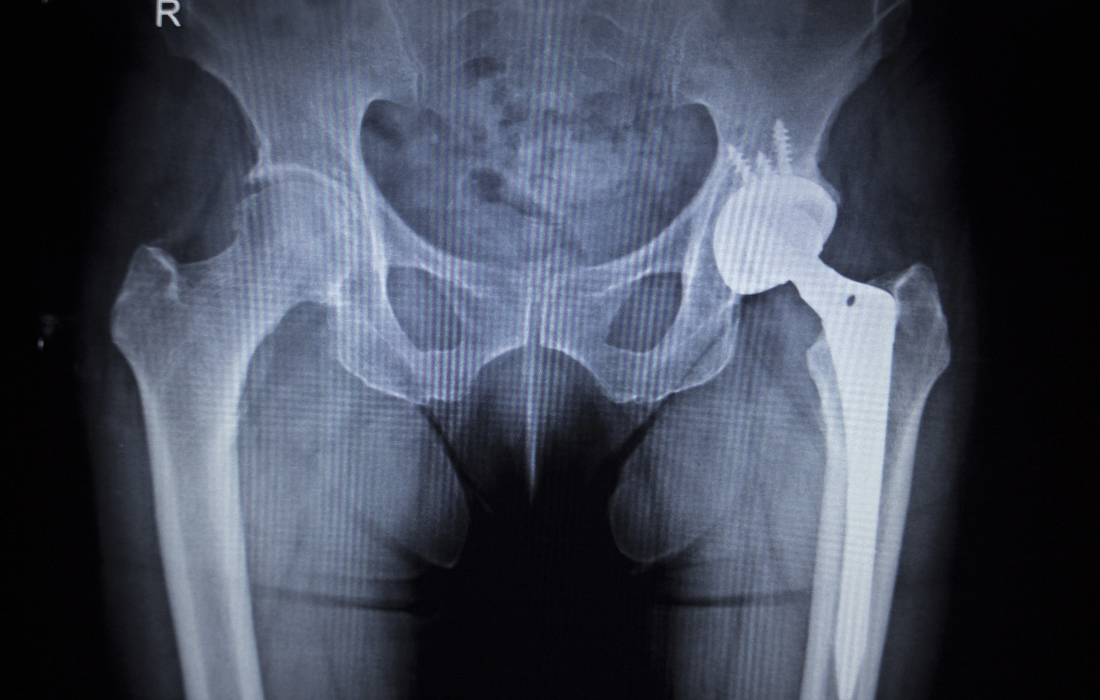
Hip surgeries, particularly hip replacements, are often presented as life-altering procedures designed to restore mobility and improve one’s quality of life. For guys, especially older guys, the idea of regaining independence through these procedures can be pretty alluring. But… the reality is, of course, not so black and white.
Hip surgeries, particularly those following hip fractures, are associated with significantly increased mortality risks. This article explores why these risks exist, why hip surgeries are so commonly recommended, and what you might consider before going under the knife.
The Relationship Between Hip Surgery and Mortality
Studies consistently show that hip fracture patients face alarmingly high mortality rates compared to the general population. For instance, a Finnish population-based study revealed that the mortality rate for hip fracture patients is three times higher than that of their age-matched peers. While the risk is most pronounced in the immediate months following surgery, it continues for years.
Cumulative mortality statistics paint a sobering picture:
- 10.5% mortality within 30 days of surgery.
- 21.5% within 6 months.
- 27.3% within the first year.
- By nine years, nearly 80% of hip fracture patients had died.
These figures underscore the need to take a serious look at the risks associated with these surgeries and the underlying factors contributing to such grim outcomes.
Why Mortality Increases After Hip Surgery
Complications Related to Surgery and Fracture
- Pulmonary Embolism: Blood clots formed during or after surgery can travel to the lungs, causing life-threatening complications.
- Infections: Post-operative infections, including pneumonia and surgical site infections, are common among older, frailer patients.
- Cardiovascular Strain: The physiological stress of surgery can exacerbate pre-existing heart conditions or trigger acute events like heart failure.
Pre-existing Conditions
Many patients undergoing hip surgery have underlying health issues that increase their vulnerability. For instance:
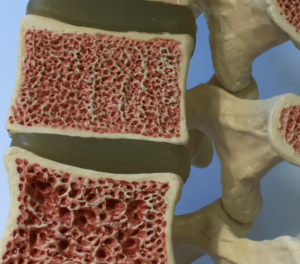
- Osteoporosis, which predisposes individuals to fractures, is itself linked to increased mortality.
- Chronic illnesses, such as diabetes or respiratory diseases, complicate recovery and increase the risk of death.

Sex-Specific Differences
- Men are at a particularly high risk. The Finnish study found that men had a 55% higher risk of death than women during the follow-up period. Contributing factors include greater frailty, more severe comorbidities, and higher rates of respiratory and circulatory system complications.
Limitations in Post-Surgical Care
- In many healthcare systems, post-surgical care for hip fracture patients is inadequate. A lack of specialized geriatric rehabilitation can lead to poorer outcomes, prolonged immobility, and secondary complications.
Why Hip Surgeries Are So Commonly Recommended
Despite the risks, hip surgeries remain one of the most commonly performed procedures worldwide. Why is this the case?
The Goals of Surgery
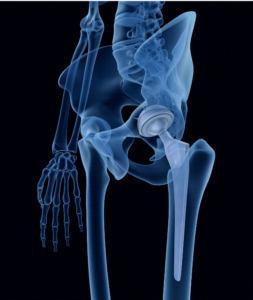
Orthopedic surgeons emphasize that hip replacements and fracture repairs can be transformative. These procedures aim to:
- Restore mobility and reduce pain.
- Prevent complications such as bedsores, muscle atrophy, and joint stiffness that arise from prolonged immobility.
- Improve quality of life, allowing patients to regain independence.
Financial and Systemic Pressures
Healthcare systems and hospitals often prioritize surgical interventions for several reasons:
- Economic Incentives: Surgeries are hugely revenue-generating procedures for hospitals and surgical teams.
- Streamlined Processes: Surgical care pathways are well-established, while non-surgical management, like physical therapy, often lacks the same level of systemic support.

Cultural and Medical Norms
Surgery is often seen as the “gold standard” for addressing hip fractures. This cultural bias, combined with limited awareness of alternative treatments, pushes many patients and their families toward surgical solutions without fully considering the risks or exploring other options.
What We Can Learn From the Finnish Study
The population-based study conducted in Finland provides valuable insights into the mortality risks associated with hip surgeries:
- Excess Mortality Across All Causes
- The study found that hip fracture patients had elevated mortality rates across all major categories, including circulatory, respiratory, and digestive system diseases.
- Sex-Specific Risks
- Men were more likely than women to die from respiratory diseases, malignant neoplasms, and circulatory system diseases.

- Factors such as smoking, which is more common among older men, and greater baseline frailty likely contribute to these differences.
- Men were more likely than women to die from respiratory diseases, malignant neoplasms, and circulatory system diseases.
- Importance of Rehabilitation
- The lack of specialized geriatric rehabilitation was highlighted as a major contributor to poor outcomes in hip fracture patients. Multidisciplinary approaches to recovery can significantly improve survival and quality of life.
Alternatives to Surgery and Preventive Strategies
While surgery can certainly be necessary for severe fractures, alternatives and preventive measures should not be overlooked, certainly not as much as they are.
Preventing Hip Fractures
- Bone Health
- Address osteoporosis naturally through calcium and vitamin D supplementation, weight-bearing exercises, and medications like bisphosphonates.
- Fall Prevention
- Home modifications (e.g., grab bars, non-slip rugs).
- Strength and balance training programs.

Non-Surgical Management
In some cases, particularly for less severe fractures, non-surgical options can be explored:
- Pain management through medications or injections.
- Physical therapy to strengthen surrounding muscles and improve mobility.
- Use of assistive devices, such as walkers or canes, to support movement.
Improving Post-Surgical Care
For patients who do undergo surgery, post-operative care is critical:
- Rehabilitation Programs: Tailored physical therapy and occupational therapy plans.
- Comprehensive Health Monitoring: Regular follow-ups to detect and manage complications early.

- Nutritional Support: Addressing malnutrition to support healing and recovery.
Navigating the Decision: Is Surgery the Right Choice?
Deciding whether to undergo hip surgery is a complex and deeply personal decision. Patients should consider the following:
- What are my specific risks for complications and mortality?
- Are there non-surgical or less invasive options available?
- What does the post-operative care plan entail?
- How will surgery impact my overall quality of life?
Balancing the potential benefits of surgery against its risks requires open and honest communication with healthcare providers. Seeking second, and even third opinions, and involving family members in the decision-making process can also provide clarity and insight.
Closing Thoughts
Hip surgeries can be life-changing, but they are not without significant risks, especially for older men with underlying health conditions. Understanding the factors that contribute to increased mortality – and the systemic pressures that make these surgeries so incredibly common – is crucial for making informed decisions. By exploring preventive measures, considering non-surgical options, and advocating for more comprehensive post-operative care, people can take a proactive approach to their health and well-being.
factors that contribute to increased mortality – and the systemic pressures that make these surgeries so incredibly common – is crucial for making informed decisions. By exploring preventive measures, considering non-surgical options, and advocating for more comprehensive post-operative care, people can take a proactive approach to their health and well-being.
Ultimately, the goal is to make decisions that prioritize both quality and longevity of life. If you or a loved one is facing a hip surgery decision, take the time to weigh all the options and ensure that the chosen path aligns with your health goals and personal circumstances.