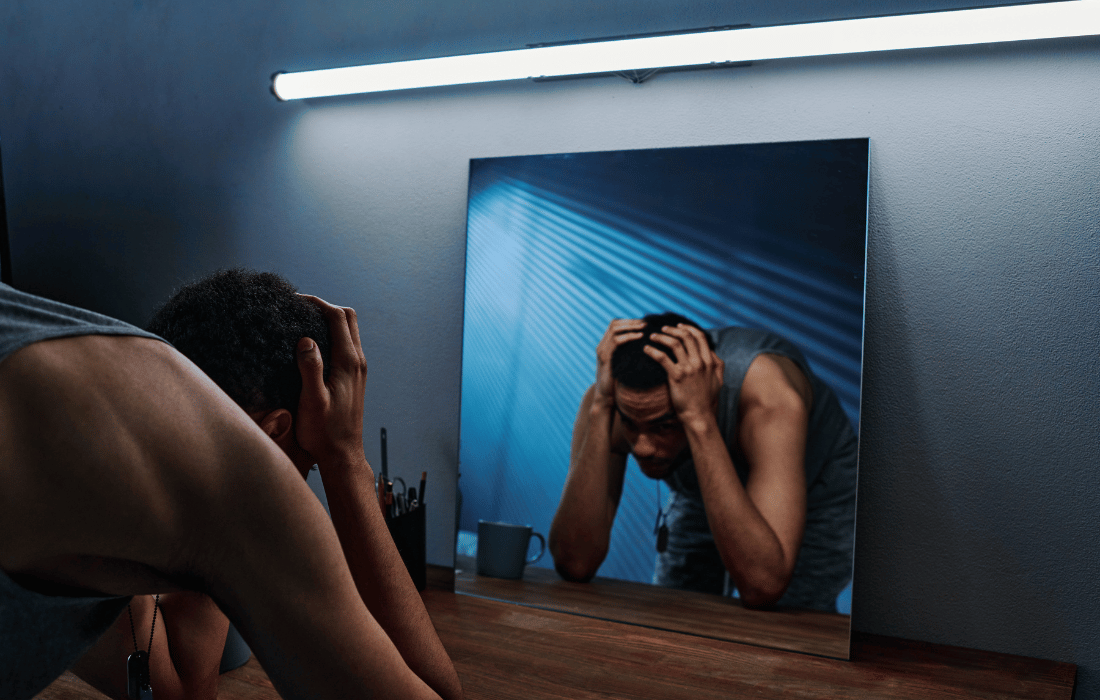
For many veterans, the battle doesn’t end when they leave the battlefield. Post-traumatic stress disorder (PTSD) and depression are incredibly pervasive issues within the veteran community, often complicated and compounded by feelings of isolation, guilt, and the challenges of reintegration into civilian life. Despite the availability of therapies like cognitive-behavioral therapy (CBT) and SSRIs, a significant number of veterans find these approaches ineffective, leaving them trapped in their cycles of despair. Enter ibogaine: a natural, plant-derived compound that is gaining attention for its remarkable potential to treat treatment-resistant PTSD and depression.
Could this alternative treatment be the breakthrough veterans have been waiting for? Let’s dive into the science, stories, and controversy surrounding ibogaine.
What is Ibogaine?
Ibogaine is a naturally occurring psychoactive substance extracted from the roots of Tabernanthe iboga, a shrub native to Central and West Africa. Traditionally used in spiritual ceremonies by the Bwiti people of Gabon, ibogaine has been revered for its ability to induce intense introspection and spiritual healing. In recent decades, researchers and clinicians have turned their attention to ibogaine for its therapeutic effects on addiction and mental health conditions.
spiritual ceremonies by the Bwiti people of Gabon, ibogaine has been revered for its ability to induce intense introspection and spiritual healing. In recent decades, researchers and clinicians have turned their attention to ibogaine for its therapeutic effects on addiction and mental health conditions.
What makes ibogaine unique is its dual action. First, it works on the brain’s NMDA receptors, which play a key role in learning, memory, and mood regulation. Second, it promotes neurogenesis – the growth of new neural pathways – which is crucial for resetting the brain’s chemistry. Unlike traditional medications, which often only mask symptoms, ibogaine addresses the root causes of trauma and offers a fresh neurological start.
Why Veterans Need New Solutions
The statistics surrounding veterans’ mental health are harrowing. According to the U.S. Department of Veterans Affairs, anywhere from 11% to 20% of veterans who served in Operations Iraqi Freedom and Enduring Freedom experience PTSD in a given year. For those who served in Vietnam, that number rises to 30%. Beyond PTSD, veterans are also disproportionately affected by major depressive disorder, substance use disorders, and suicide.
Many veterans report that traditional treatments fail to provide relief. SSRIs, while widely prescribed, can take weeks to take effect – if they work at all – and often come with debilitating side effects. Similarly, therapies like CBT require sustained effort and emotional readiness that can feel out of reach for those in the depths of despair.
For veterans caught in this cycle, ibogaine represents a lifeline. Its rapid action and profound psychological effects make it a compelling option for those who feel they’ve run out of hope.

How Ibogaine Works
Ibogaine’s effects are both physiological and psychological, making it uniquely suited to address the complexities of PTSD and depression.
Resetting Brain Chemistry
Ibogaine acts on multiple neurotransmitter systems, including serotonin and dopamine, to rebalance brain chemistry. For individuals with PTSD, this “reset” can alleviate hyperarousal and intrusive memories, while also reducing the depressive symptoms that often accompany trauma.
Facilitating Introspection
The hallucinogenic properties of ibogaine induce a dream-like state that allows users to confront buried memories and emotions. This process often leads to a profound sense of understanding and closure, which can be transformative for veterans processing wartime trauma.
Breaking Addictive Cycles
Many veterans with PTSD turn to alcohol or drugs as a coping mechanism. Ibogaine has been extensively studied for its ability to interrupt addictive behaviors, offering a twofold benefit for those struggling with co-occurring disorders.
Why Big Pharma Hates Ibogaine
If ibogaine is so promising, why isn’t it already mainstream? And why is it classified as an illegal Schedule 1 substance along with heroin? The answer lies in the powerful influence of the pharmaceutical industry.
Threat to Profits
Big Pharma thrives on lifelong customers. Medications like SSRIs, benzodiazepines, and other psychiatric drugs generate billions of dollars annually. Ibogaine, on the other hand, is a one-time or short-term treatment with lasting effects, meaning it doesn’t provide the continuous revenue stream that pharmaceutical companies rely on.
No Patent, No Profit
Because ibogaine is a naturally occurring substance, it cannot be patented in the same way synthetic pharmaceuticals can. This makes it an unappealing investment for pharmaceutical giants, who prefer to fund research on drugs they can monopolize.
Disrupting the Current Mental Health Model
The existing model of mental health treatment is built around symptom management rather than true healing. Long-term dependency on medications is the norm, whereas ibogaine’s potential to provide a lasting reset threatens this entire system.
Regulatory and Political Roadblocks
Pharmaceutical companies wield immense lobbying power. The classification of ibogaine as a Schedule I substance – meaning it’s deemed to have no medical value – is largely due to outdated policies and pressure from industries that benefit from maintaining the status quo.
Evidence Supporting Ibogaine for PTSD and Depression
Though still in its early stages, research on ibogaine’s therapeutic potential is promising.
- Clinical Trials: A growing body of studies highlights ibogaine’s efficacy in treating addiction, with secondary benefits for depression and trauma-related symptoms. For instance, a 2017 study published in the American Journal of Drug and Alcohol Abuse found that a single dose of ibogaine significantly reduced withdrawal symptoms and cravings in individuals with opioid use disorder.
- Case Studies: Veterans who have undergone ibogaine therapy report life-changing results. Many describe it as a transformative experience that allowed them to process trauma in ways traditional therapy could not.
- Neurobiological Evidence: Studies on animals and humans suggest that ibogaine’s effects on brain plasticity could make it a powerful tool for treating conditions rooted in dysfunctional neural pathways.
Current Access and Advocacy
Despite the challenges, the data and case studies are undeniable and access to ibogaine therapy is slowly improving. A number of clinics around the world cater specifically to veterans, offering tailored treatment plans that address both mental health and addiction. Organizations like Veterans for Entheogenic Therapy (VET) and Veterans Exploring Treatment Solutions (VETS) are working tirelessly to raise awareness and push for policy changes that would make ibogaine and other psychedelics more accessible in the U.S.
A Path Forward
The potential of ibogaine to revolutionize PTSD and depression treatment is immense, but its integration into mainstream healthcare will require significant investment in research, education, and advocacy. Here are some steps forward:
immense, but its integration into mainstream healthcare will require significant investment in research, education, and advocacy. Here are some steps forward:
- Funding Clinical Trials: More robust studies are needed to solidify ibogaine’s safety and efficacy.
- Policy Reform: Advocating for the reclassification of ibogaine to enable its use in therapeutic settings.
- Veteran Advocacy: Continued support for organizations championing alternative therapies for veterans.
Conclusion
For veterans battling treatment-resistant PTSD and depression, ibogaine offers a beacon of hope. By addressing the root causes of trauma and promoting profound psychological healing, this plant-derived compound could redefine what’s possible in mental health care. While there are certainly still some challenges, the stories of transformation and emerging research are too compelling to ignore. With continued advocacy and scientific exploration, ibogaine could one day become a cornerstone of holistic healing, particularly for those who have given so much in service to others as our veterans have.