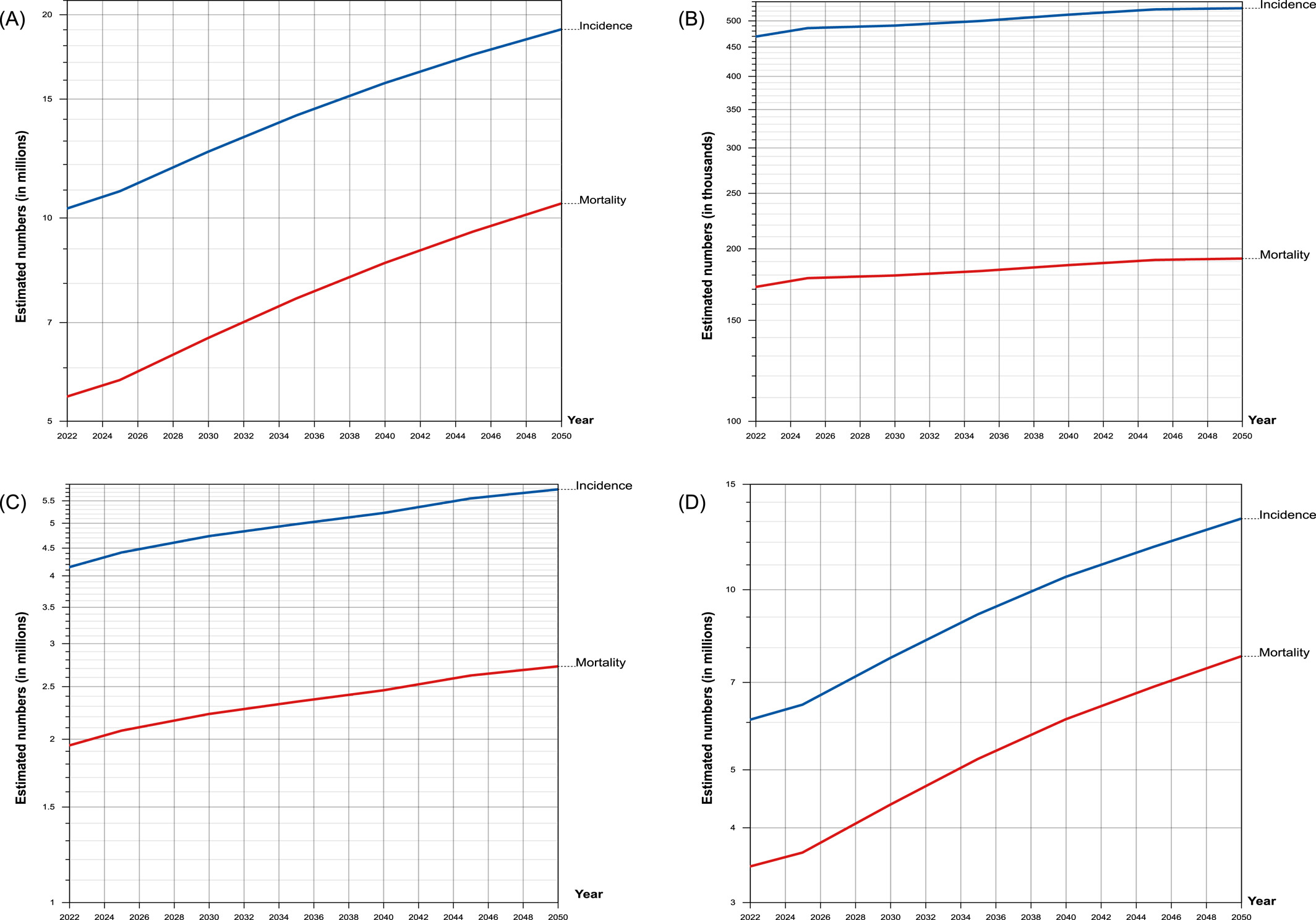
A massive surge in global cancer rates among men is quietly underway. According to a groundbreaking study published in Cancer (August 2024), male cancer cases are expected to rise by over 84% by 2050, with deaths increasing by a shocking 93%. These numbers are not just abstract predictions—they represent real people, real families, and a future public health crisis if no action is taken.
To put that in perspective, over 10 million men were diagnosed with cancer in 2022. By 2050? That number is projected to hit 19 million. Deaths will jump from 5.4 million to 10.5 million. The study, which examined data from 185 countries and 30 different cancer types, revealed a dark truth: men are disproportionately affected, more likely to die, and less likely to receive preventive care or early diagnosis.
And the scariest part? Most of this increase is preventable.
So, what’s behind this dramatic increase? And more importantly, what can we do about it?
Why Are Men at Greater Risk?
Understanding the reasons behind the surge in men’s cancer rates starts with examining the unique vulnerabilities men face. From lifestyle factors to screening gaps, a perfect storm of risk converges on the male population globally.
1. Behavioral and Environmental Risk Factors
Men, as a group, tend to exhibit higher rates of behaviors associated with cancer risk:
Smoking: As of 2020, 32.6% of men worldwide smoked compared to just 6.5% of women.
Alcohol consumption: Men drink more frequently and heavily, which increases cancer risk across multiple organ systems.
Occupational exposure: Men dominate high-risk industries such as mining, construction, and manufacturing, where exposure to carcinogens is more common.
Poor diet and lifestyle: Processed foods with seed oils, lack of physical activity, sleep deprivation, and chronic stress are all modern-day cancer triggers that are disproportionately seen in men.
These factors are modifiable. But awareness, access to care, and cultural norms around masculinity often delay prevention and treatment.
2. Lack of Male-Specific Screening Programs
Women benefit from widespread breast and cervical cancer screenings. For men, prostate, testicular, and colorectal screenings are less emphasized, less accessible, and sometimes poorly promoted. This leads to late-stage diagnoses when survival odds are much lower.
In many countries, there’s still no national policy or funding for regular PSA testing or educational campaigns for testicular cancer. Even among those with insurance, men may not feel empowered to request these tests unless symptoms are already noticeable.
3. Biologic and Health-Seeking Differences
Beyond lifestyle, biologic differences may play a role in why men experience worse outcomes. Hormonal differences, immune response variations, and how men metabolize toxins can influence risk. Additionally, men are less likely to seek medical attention early, often ignoring symptoms until the disease has progressed.
A 2021 survey found that 65% of men delay visiting the doctor as long as possible. Many cited reasons such as not wanting to seem weak, being too busy, or believing the symptoms would go away.
The Numbers Don’t Lie: Global Trends in Men’s Cancer
Men aged 65+ will see the biggest surge in cancer cases. Between 2022 and 2050:
Cancer cases in older men will increase by 117%
Cancer deaths in this age group will jump by 124.5%
As longevity increases globally, chronic diseases like cancer are taking center stage. This means more men are living long enough to develop cancers that might not have shown up in previous generations.
But are we ready for this silver tsunami of male cancer patients? Not even close.
Global Inequities: Where You Live Matters
There is a stark disparity between countries with high and low Human Development Index (HDI):
Low-HDI countries will see a 138% rise in cases and 141% rise in deaths.
Very-high-HDI countries are projected to see increases of 50% (cases) and 63.9% (deaths).
That means poorer countries will bear the brunt of the burden, with less access to diagnostics, treatment, or preventive services. Many low-HDI countries don’t even have consistent access to cancer registries, basic imaging tools, or chemotherapy agents.
Disproportionate Impact on Working-Age Men
Between 2022 and 2050, men aged 15 to 64 will see a 39% increase in cancer cases and a nearly 40% rise in deaths. That’s a devastating blow to the global workforce and economies.
Imagine the ripple effect:
Families losing providers
Companies losing skilled labor
Healthcare systems collapsing under demand
And many of these men will be in the prime of their lives—fathers, sons, entrepreneurs, builders, and leaders.
Which Cancers Are Driving This Surge?
Not all cancers affect men equally. Some are far more common, some more deadly, and many are deeply tied to preventable risk factors. Understanding which types are fueling this surge is key to stopping it.
The Top Killers in Men:
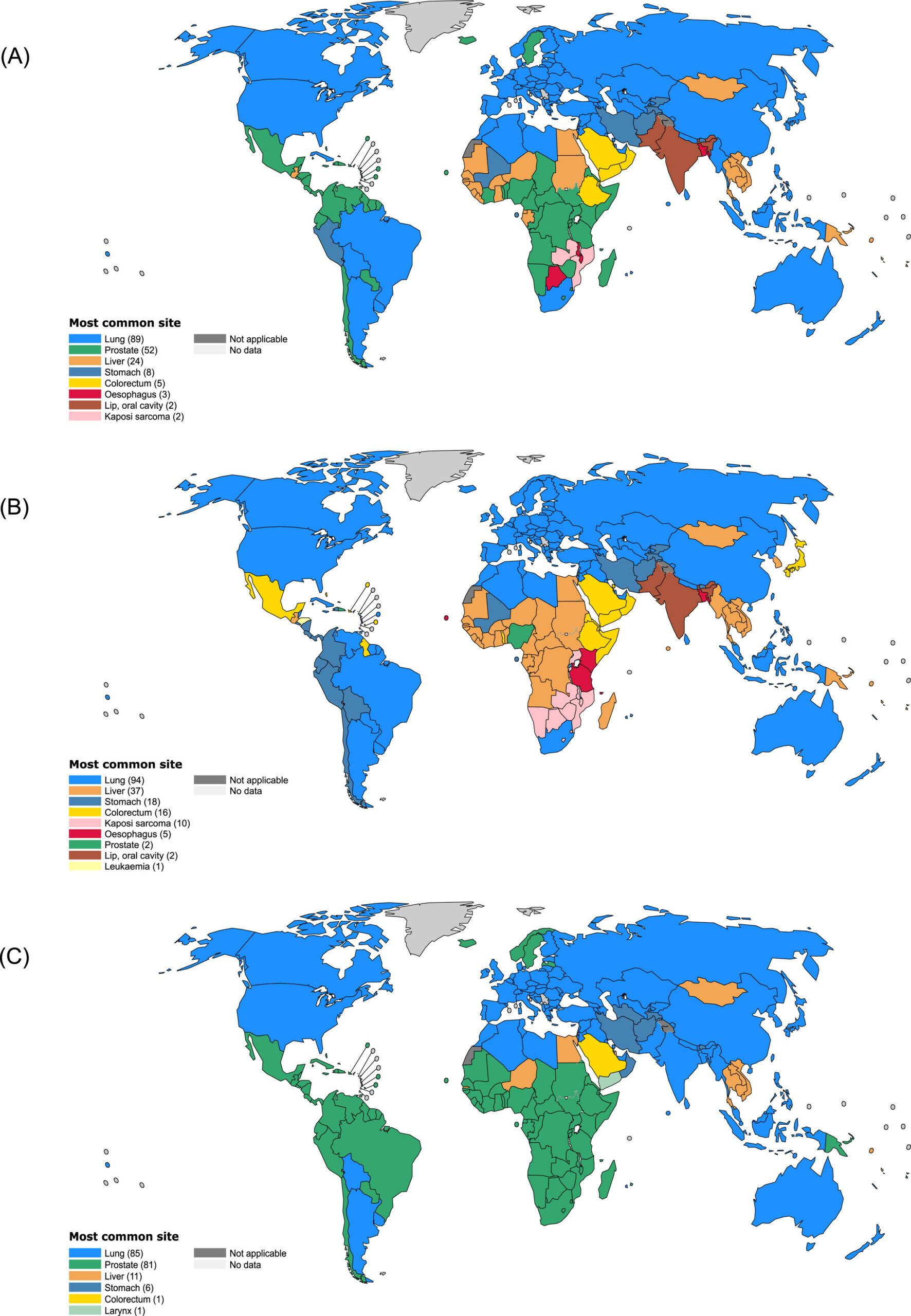
Lung cancer: Continues to be the leading cause of cancer death across all age groups. Smoking, pollution, and occupational exposures are key contributors.
Prostate cancer: The most diagnosed cancer in men across two-thirds of countries. While it has a relatively low MIR in high-HDI countries, it’s a different story elsewhere.
Colorectal cancer: Increasingly common in men under 50. Diets high in processed foods, alcohol, and a lack of fiber are major culprits.
Liver and esophageal cancers: Often tied to alcohol, hepatitis, and aflatoxins. These have among the highest fatality rates due to late detection.
Pancreatic cancer: A rare but deadly cancer with a 90.9% MIR. Often asymptomatic until it’s too late.
Rare but Deadly: The Hidden Threat
Men are also more likely to suffer from workplace-related cancers like mesothelioma (linked to asbestos) and bladder cancer (linked to industrial chemical exposure).
And in some regions, cancers like Kaposi sarcoma and testicular cancer are increasing due to HIV prevalence and poor awareness, respectively.
Mortality-to-Incidence Ratio: What It Truly Tells Us
MIR is a powerful indicator of survival odds. A high MIR = more deaths per diagnosis. In 2022:
Global average MIR among men: 54.9%
Pancreatic cancer: 90.9% MIR
Liver cancer: 85.8% MIR
MIR tells a grim story of where cancer hits hardest and where systems are failing.
Countries with lower HDI had significantly higher MIRs. For example:
The Gambia: 86.6% MIR
Norway: 28% MIR
This reflects both late diagnoses and limited treatment infrastructure.
What Can Be Done: A Roadmap to Prevention and Equity
The numbers are daunting, but they’re not destiny. With targeted efforts, cultural shifts, and smart policy changes, we can reverse this trend and rewrite the future of men’s health.
1. Early Detection and Male-Specific Screening
We must normalize:
Annual prostate-specific antigen (PSA) testing
Testicular self-exams for men under 40
Colorectal screenings starting at age 45, or earlier if there’s family history
And globally, we need to fight for more equitable access to:
Imaging equipment (MRI, CT, PET)
Skilled professionals and pathology labs
Surgical and radiation therapy infrastructure
2. Tackle the Risk Factors at the Root
The foundation of cancer prevention lies in addressing the everyday habits and exposures that quietly shape our health. For men, these risk factors are often cultural, environmental, and deeply ingrained—but change is possible.
a. Stop Normalizing Toxic Habits
Cigarette smoking and vaping remain a global killer. Men must be the target of hard-hitting anti-smoking campaigns.
Alcohol use, particularly in binge form, needs more cultural scrutiny.
Encourage physical activity, sunlight exposure, and quality sleep
Shift from ultra-processed diets to real food: grass-fed meats, organic produce, and clean fats
b. Workplace Safety
We must implement:
Safer practices in construction, manufacturing, and agriculture
Regular monitoring of exposure levels to pesticides, EMFs, heavy metals, etc.
Government accountability for industrial carcinogens
3. Global Health Investment
To prevent a massive rise in cancer deaths, the study calls for:
Universal health coverage, particularly in low-HDI countries
More publicly funded medical schools and trained specialists
Stronger infrastructure for diagnosis and radiation therapy
National and international collaborations to share knowledge and resources
This includes platforms for:
Data sharing and cancer registries
Training physicians from low-HDI countries in global centers
Subsidized medication and equipment distribution
Focus on Men’s Health Culture
Men are less likely to talk about their symptoms. Less likely to visit a doctor. Less likely to take preventive action. These cultural norms must change.
We need male-specific health campaigns, mental health support, and community programs that de-stigmatize care and encourage action.
Changing the culture means teaching boys early that strength isn’t about silence. It’s about courage—the courage to care for yourself.
How to Protect Yourself: Actionable Takeaways
Prevention isn’t just about luck or genetics—it’s about taking ownership of your health. These steps are simple but powerful ways to reduce your risk and stay ahead of the rising cancer curve.
1. Get screened
If you’re over 40, ask your doctor about PSA, colonoscopies, and full blood panels. Even basic checkups can catch cancer in time.
2. Stop smoking (now)
This one speaks for itself. Your lungs (and loved ones) will thank you.
3. Clean up your environment
Avoid toxins at work, home, and in your food. Eat clean, organic when possible. Use glass instead of plastic. Say no to synthetic air fresheners and endocrine-disrupting fragrances. Protect yourself from harmful EMFs coming from wireless radiation sources.
4. Be your own advocate
No one cares more about your body than you do. Don’t wait for symptoms to become emergencies.
Ask the hard questions. Do your research. And push back when something doesn’t feel right.
5. Support systems that support men
Whether it’s donating to men’s health nonprofits, sharing educational materials, or lobbying for policy changes, we all have a role to play.
Final Thoughts: The Clock Is Ticking
The science is clear. If nothing changes, millions more men will die needlessly of preventable or treatable cancers.
But it doesn’t have to be this way.
We need action, not just from governments and health organizations, but from every man reading this. Speak up. Get checked. And help shift the narrative around men’s health from silent suffering to empowered action.
Because when men thrive, families thrive. Communities thrive. Societies thrive.
Cancer is coming. But we still have time to fight back.